New mRNA Cancer Vaccine: A Promising Treatment Against Tumors

Research regarding cancer treatment has gradually improved over the years, expanding the range of effective intervention methods: From tumour removal surgery and radiation therapy to targeting rapidly growing cells with chemotherapy. Now, thanks to ever-expanding research, scientists have come up with another treatment that has proven more effective than the methods mentioned above. Namely, immunotherapy, which is an effective practice of targeting tumours with more precision than ever before.
What Does Immunotherapy Imply?
Immunotherapy works by helping the immune system in our bodies recognise and attack cancer cells. The first standardised cancer immunotherapy treatment was developed by William B. Coley in 1891 in which the so-called "Coley Toxin", developed from Streptococcal bacteria, was used to treat patients with bone and soft tissue sarcomas. The stimulated immune system responses shrank the tumour significantly. Coley's research, which ended in 1933, paved the way for cures and positive treatment outcomes for liver cancer, cervical cancer, colon cancer, melanomas and bladder cancer, among others.
On the topic of immunotherapy, there are several types, including monoclonal antibodies, checkpoint inhibitors and vaccines.
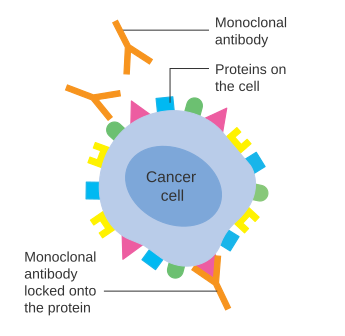
Antibodies exist naturally in our blood and help the body fight infection. Monoclonal antibodies (MABs) are made artificially and mimic the function of natural antibodies. The term "monoclonal" means all one type, implying that each MAB therapy contains many copies of one type of antibody. The main function of MABs, is to identify and bind to specific proteins found on the surface of cancer cells. After doing this, they send a signal to the immune cells. The immune cells arrive and punch holes in the cancer cell, causing it to die. This process is called antibody-dependent cell-mediated cytotoxicity. (ADCC)
Examples of MABs that undergo this process include rituximab, used to treat chronic lymphocytic leukaemia; cetuximab, used to treat advanced bowel cancer; and trastuzumab, used to treat breast cancer and stomach cancer.
Other MABs work by acting on the cells of the immune system, rather than directly targeting cancer cells. An example of this is checkpoint inhibitors which block proteins that prevent the immune system from attacking cancer cells. Said proteins help regulate the body's T-cells, these cells are responsible for both activating and terminating immune responses with the help of checkpoint proteins. If, for example, an infection is present, a checkpoint protein will signal to the T-cell to activate. However, if the T-cell is activated for too long, they can start to destroy healthy cells and tissues. Since cancer cells make high levels of protein, they can switch off T-cells, making them unable to recognise and kill cancer cells. The checkpoint inhibitor's job is to block the high levels of protein emitted from cancer cells to prevent this from happening.

Patients usually receive MAB treatment through a drip into a vein, known as an infusion. Although some treatments may require an injection under the skin, known as a subcutaneous injection. The frequency and quantity of treatments depend on the MAB type as well as the type of cancer.
While each of these approaches uniquely targets tumours to stop their growth or even kill the cancerous cells, they come with their own limitations. Firstly, these immunotherapeutic practices involve targeting only a singular antigen on tumours. Secondly, they do not provide long-lasting immunity against the potential development of future tumours, which opens the possibility of the tumour escaping and re-emerging once therapy stops. Luckily, vaccines against cancer offer a potential solution to both problems.
Cancer Vaccines - Preventative or Therapeutic?
Cancer vaccines have been of interest to researchers since the 1990s. Though actually implementing immunotherapy in cancer treatment has proven to be challenging due to limited knowledge and resources.
There are two varieties of cancer vaccines: preventative and therapeutic. Currently approved preventative cancer vaccines include the hepatitis B vaccine and human papillomavirus vaccine, both of which provide immunity against specific viruses that can cause cancer after infection. In contrast, developing a preventative vaccine against spontaneous tumours is another task entirely. It is impossible to predict when or how a mutation will occur in a cell to manifest a tumorigenic protein against which to formulate a vaccine. Instead, it is more likely to create a model of vaccination that can be used therapeutically to treat already-existing tumours.
The way a therapeutic cancer vaccine works is that it introduces the immune system to one or more tumour antigens, thus prompting the immune cells to activate against the antigens, which in turns enables them to target and destroy the tumour. An antigen is any substance that causes the body to make an immune response against it. Antigens include toxins, bacteria, viruses and cancer cells.

The first step in doing this is delivering the antigens to immune cells, specifically dendritic cells. There are several different approaches when it comes to this. One way is deliver antigens that are shared by many people with the same type of cancer. Another way is to make use of messenger RNA (mRNA) technology by taking a sample of an individual patient's tumour to produce personalised neoantigens expressed exclusively by tumour cells and not by any of a patient's healthy cells. Other methods involve injecting dendritic cells that are pre-loaded with cancer antigens or generating antigens inside the body and promoting their uptake by dendritic cells.
Once they receive the antigens, dendritic cells bind and activate CD8 cytotoxic T-cells, which then mount an attack on the tumour. For maximal effect, dendritic cells also stimulate CD4+ 'helper' T-cells which aid in the activation of CD8+ T-cells and cell memory. These T-cells have the capacity to destroy even large tumours, but cancer cells can acquire ways of evading immune attacks. They can do this by reducing their antigen expression to hide from immune cells, and instead express molecules - such as the checkpoint protein PD-L1- that inhibit tumour-attacking T-cells. This poses a problem which must be overcome in order for immunotherapies to reach their full potential.
Treatment of Pancreatic Cancer, Phase-1 Trial Results
An experimental approach to treating pancreatic cancer with an mRNA-based therapeutic cancer vaccine showed the potential to stimulate an immune response that may reduce the risk of the cancer returning after surgery.
The trial involved studying 16 Memorial Sloan Kettering Cancer Center (MSK) patients who received autogene cevumeran (mRNA vaccine), an immunotherapy drug called atexolizumab and a chemotherapy treatment plan called mFOLFIRNOX. The mRNA cancer vaccines were curated based on the mutational profile of each individual tumour, thus teaching T-cells to recognise neoantigens that are found exclusively in each patient's pancreatic tumour.
Results from the phase 1 clinical trial showed that the vaccine activated immune cells that persisted in the body up to three years after treatment in 8 patients. 6 of these patients had not seen their cancer return and the other 2 patients relapsed. Tissue and blood samples were taken from the 8 patients. Upon studying them, researchers found that 98% of the T-cells specifically activated by the cancer vaccines were not present before vaccination. On top of that, more than 80% of the vaccine-induced T-cells persisted 2-3 years after treatment. This information suggests that the cancer vaccines stimulated a durable T-cell response.
On the other hand, the cancer returned in 7 of the 8 patients whose immune systems had not responded to the vaccine during the study period. Even with this information, researchers are not yet sure if there is indeed a correlation between the vaccine and the delay in cancer recurrence.
What is evident, however, is the fact that the treatment plan helped half of the participants. This is very promising as pancreatic cancer is one of the deadliest cancers. Even with surgery and other treatment plans, only about 12% of patients survive five years after diagnosis.
There is still much left to uncover regarding cancer vaccines; Which is why the researchers are conducting a follow-experiment which began in July 2023. This study will involve approximately 260 patients around the world. Researchers are investigating whether the mRNA method works better than the current standard treatment for pancreatic cancer.
The control group will receive standard treatment: surgery followed by chemotherapy. Meanwhile, the other group will receive the experimental treatment: surgery followed by autogene cevumeran, a checkpoint inhibitor immunotherapy drug as well as chemotherapy. The mRNA vaccines will be custom-made for each patient and given in two doses. One dose at the beginning of the treatment and one dose later on to provide a boost.
There has been great interest in using immunotherapy for pancreatic cancer because nothing else has worked very well. We thought immunotherapy held promise because of research we began about eight years ago. A small subset of patients with pancreatic cancer manage to beat the odds and survive after their tumor is removed. We looked at the tumors taken from these select patients and saw that the tumors had an especially large number of immune cells in them, especially T cells. Something in the tumor cells seemed to be sending out a signal that alerted the T cells and drew them in. - Memorial Sloan Kettering Cancer Center (MSK) pancreatic cancer surgeon-scientist Vinod Balachandran, MD.
Conclusions
According to Cancer Research UK, the lifetime risk of being diagnosed with cancer is nearly 1 in 2 (43%) for females and nearly 1 and 2 (45%) for males born in 1961 in the UK. While these statistics can vary depending on where in the world you are, they are undeniably alarming. This is why the recent successes of mRNA cancer vaccines have been met with such hopeful optimism. The future of cancer research appears promising, but even more so is the hope held by those diagnosed with cancer or those who have loved ones affected by the disease.



